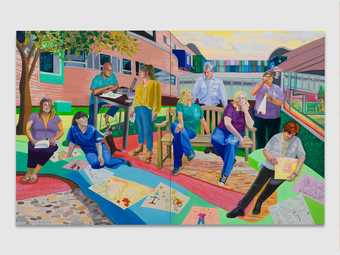
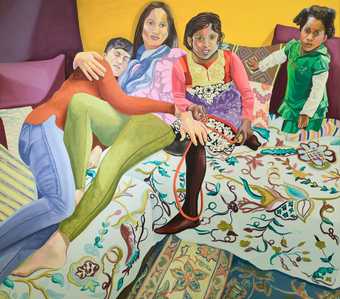
Aliza Nisenbaum Naveena, Student Nurse and Succulents 2020 © Aliza Nisenbaum. Photography by Jeff McLane, courtesy the artist and Anton Kern Gallery, New York
Influenced by the Mexican mural movement and its depiction of social history, Aliza Nisenbaum creates colourful paintings that often focus on community groups. She believes that ‘paying attention can be a political act’ and usually spends hours with her sitters, painting them from life while developing a personal connection through conversations that enable her to highlight their individuality.
In recent months, Nisenbaum has worked in response to the current global health crisis, focusing her attention on NHS staff from the Merseyside region whose work has proven vital during the Covid-19 pandemic. This exhibition includes 2 newly commissioned group portraits and 11 individual watercolour paintings, as well as a selection of works from the last 5 years that reflect on ideas of togetherness, belonging and diversity. Nisenbaum’s new paintings capture the stories of these frontline NHS workers and highlight the impact that Covid-19 has had on their work and home lives. They are shown alongside things that have given them support and hope through this difficult time, such as pets or musical instruments.
Nisenbaum has worked with these sitters remotely, painting from life via video chat, even though the pandemic has prevented her from travelling to the UK. Selected through an open call, the people depicted in these new works represent a broad range of care workers, including doctors, nurses, porters, researchers and healthcare assistants. The paintings are complemented by images of flowers, offered by Nisenbaum as a gesture of thanks to NHS staff who work tirelessly for their community.
We have highlighted the stories of all the local healthcare workers who posed for Nisenbaum, written in their own words. These powerful and at times emotional accounts detail how Covid-19 has affected every one of them.
All works by Aliza Nisenbaum, born 1977 Born Mexico, works US
Sitter captions
Alan, Student Nurse
I was close to finishing my nursing degree when Covid first hit. Initially the university closed, but healthcare students could apply for NHS placements, to help with the pandemic while completing our qualifications. After 6 weeks of waiting, I got the call to confirm my placement. I was so happy, as this was the last thing I needed to complete in order to qualify as a nurse!
At this time, my mother was seriously ill in hospital. The day before I was due to start my placement, my sister phoned me to say that my mum’s ventilator settings were being lowered, which I knew wasn’t good. Myself and my dad went straight to the hospital, where we met my two sisters. The nurse looking after my mum explained what was happening. I held my mum’s hand as I looked at her monitors and I could see her heart rate become erratic, then I noticed that there was a long pause on her ventilator, and I knew that she had passed away. The feeling was one of true loss, a different kind of pain that I’d never felt in my life.
I still went to my placement induction the next day, as I knew my mum would have wanted me to, and I wanted to make her proud. She raised me to never give up, and whenever I had setbacks, she was always there to pick me up and give me the strength to carry on. When I woke up on the first morning of my placement, I noticed her hairbrush and I put some of her hair in a locket, so that I could always keep part of her close to me. I’ve since finished my qualifications, and I work as a nurse at the Walton Centre.
Reverend Jackie, Hospital Chaplain
The job of a chaplain is all about support, whether it’s listening to somebody, or allowing people the freedom to cry, scream, or shout. During the pandemic it has been very difficult because we often physically couldn’t go and see patients and their relatives. It wasn’t necessarily only people of faith, it’s everybody – although I’ve found a lot of people have come to faith during this, especially when they had lost somebody. It brought comfort, to feel that their loved one was resting in heaven and not in any pain. Some people lost quite a few loved ones, that was heart-breaking. Patients in the past have asked me for a hug, and I’m a hugger, but now physical contact is not allowed which is very difficult. You couldn’t even hold someone’s hand.
The people I saw were mostly staff, who needed a tremendous amount of support as well. A lot of them were separated from their families and they were scared, they were exhausted. For them to have someone there who they could just come and talk to was important. Their life was being in work all the time, so to be there for them was really quite a privilege.
I was really struck by the care that came out of society during this time. I hope, I really pray, that that will continue afterwards.
Emily, Critical Care Nurse
I was working as a critical care nurse and during the Covid pandemic we converted our unit into an intensive care unit. It was challenging because we don’t usually look after those types of patients, but we had to. We had ventilator patients on the unit for about two months, which was a very intense time. We did 12-hour shifts, and I ended up on 6 weeks of night shifts. Nothing resembled normality. Everyone was wearing full PPE; you couldn’t recognise anybody. We would wear PPE for 4 or 5 hours at a time, without eating or drinking, or going to the bathroom, because you were aware of not wanting to use extra PPE if you had to take it off.
Through most of it I was running on adrenaline, it’s only now that I’ve got time to process it. Now there are a lot of us who experience trauma, like flashbacks and emotions that are very close to the surface. Of course, it was horrible, but I was glad to be able to be a part of it and do something. I was very proud of our unit and how well everybody adapted, our team spirit and our camaraderie.
Stephen, Orthoptist
I work as an Orthoptist which is an eye specialist in vision and eye movement disorders, and I work with both children and adults. We always try to make the hospital appointments as fun as we can for the children, which is even more important during this confusing and scary time. Though my colleagues and I now have to wear full PPE which can be distressing for kids, the children see it as playing games rather than getting tests. I create a certificate of bravery for each child which I then email to the parents after their appointment. I ask them what their absolute favourite character/cartoon/film and colour is and then create a certificate around this. Some of the parents have told me how much it’s meant to the children to get their certificate. Something so small can be so important.
In addition to this job I am a yoga teacher – my husband Paul, and I, run our own yoga business. This has changed completely since lockdown – we now run our classes online via Zoom. Many have said it’s been a lifeline to them, but it truly has been to us too. To be able to still connect and keep some normality during this time has been amazing.
Colin, Nursing Lecturer
I was teaching part-time in a university when the pandemic started. There was a drive from the NHS with the slogan ‘Stand up, step forward, save lives’ to encourage medical staff, initially retired people, to return to work. When this campaign came out, I thought I need to go and do something, I need to be a part of it.
My background is as an ICU nurse, but I have ended up working in all the general wards in the hospital. For someone who is used to working one-on-one, to suddenly be thrown into a situation where you are treating 30 Covid patients while wearing full PPE, was very different. I had to start re-learning everything and find things out as we went along. Many NHS staff were redeployed into the acute areas from other departments and were in a similar situation. To start with it was all a bit ‘the blind leading the blind’. I’m lucky, because my academic background is in health psychology, so I’ve got an awareness of how to take care of myself during a time like this. While I haven’t felt the need for any formal intervention or psychological support, it has been helpful to have great people around me who are very supportive.
Shari, Intensive Care Nurse
Nobody expected this pandemic. It has brought a lot of bad, but we’ve also seen a lot of good in people. The theatre staff came to help us. Everyone came together during the peak, we had to rely on each other. I imagine it was difficult for them because it’s a totally new area and experience, but they just plunged in. We just had to put one foot in front of the other, get through the day and then do it all over again the next day. But we were all like a big family and somehow, we got through it.
It was a very humbling experience, but also terrifying because every day you are confronted by your own mortality, as you don’t know if you are going to get it, no matter how careful you are. Both my partner and I are from the Philippines. When we went there on holiday earlier this year, my partner wasn’t able to travel back with me due to the travel ban, and our adopted daughter who still lives in the Philippines wasn’t able to visit. I was here alone during the peak, but I was so thankful that they were safe, and I didn’t have to worry about infecting anyone.
Now that the second wave is here, we’re doing it all over again.
Calum, Professor of Outbreak Medicine and member of SAGE
I am one of thousands of people who are part of the research attempt to beat this virus. In previous outbreaks, clinical researchers have been deeply frustrated by our inability to mount a rapid response. A group of us set up a global organisation called ISARIC in 2011 which identified the need to set up hibernating research studies in readiness for a future outbreak. Previously it took at least three months to activate a study. For Covid-19 it took one phone call because of our preparations. We were able to recruit the very first cases here and in other countries. For over 70% of people that were hospitalized with Covid-19, we know their age, sex, and ethnicity, what treatment they needed in hospital, and sadly what happened to them. It’s a privilege to have that information, but also a burden because you see what this horrendous virus is doing to people. At the start of the outbreak I could see that it was killing one in three people that came into hospital, and many people were saying this is nothing to worry about. Now, thanks to research and improved care, we have reduced deaths by half.
I’m often the person that’s bringing bad news to the public and there are many people that don’t want to hear it. We’ve got to persuade people that we are working for their wellbeing and that life will get better.
Naveena, Student Nurse
I am a student nurse within mental health, and I also work as a support worker for people with learning disabilities. My mother is an ICU nurse at Alder Hey, both my sisters are student nurses and several of my aunts also work in healthcare.
At the start of the pandemic, student nurses were asked if they would work on the front line to help out, and we all decided to volunteer for this. My twin sister worked on a Covid ward, and my younger sister worked on a critical care ICU, while I opted into a mental health ward. Because I lived in the same house with my mother and younger sister, we were all concerned about bringing the virus back home. My twin sister was working further away, and as she was working directly with Covid patients I was very worried about her being directly affected. We had never been apart for that long so that was incredibly difficult.
I was supposed to finish my nursing degree at the end of July, and I had planned to go traveling. Unfortunately, due to the pandemic my plans changed quite radically, but hopefully I can travel when this is all over.
Jessica, Student Nurse
I’m training to be a nurse, and I was on placement at a hospital at the start of the pandemic. As there is a huge shortage of nurses I decided to keep working, and it was a proper learning experience. The clapping for the NHS on Thursday evenings was amazing. I loved it, but there is not enough government support for staff working on the ground. It was hard to hear that nurses would not be given a pay rise, because as nice as the clapping was, it won’t pay the bills.
My nan is my inspiration, in the 1950s she married a Nigerian man while living in a very white, industrial mining town, so I salute her for her bravery. They had three children, including twins, but he left her, so she had to raise them by herself. Like me, she went back to college to study nursing at a slightly older age, while taking life drawing classes in the evenings. She inspired me to become a nurse, and she, along with my eldest daughter who is a budding artist herself, is the reason I wanted to take part in this project.
Ryan, Respiratory Doctor in Training
I’m a junior doctor training in respiratory medicine currently doing research, which I’ve been doing for a couple of years, up until March, when everything changed. The research I’d been working on was halted and I was called in to help out. So pretty much the next day, I was back on the wards. It was stressful because at the time, the tests we had took about four days for the results to come back, so you had to be really careful and assume that everybody had it. I remember our first patient who tested positive, I frantically thought ‘What interaction have I had with them? How much risk have I put myself at?’
Our son was born in mid-May. In March, when the outbreak really began, my wife was around twenty-six weeks pregnant, so she was isolating at home. I was going to work, so I had to be extra careful. As soon as I got home, I would take off all my clothes, run upstairs and shower, making sure I didn’t touch anything.
Ann, Nurse
I’ve been a nurse for a lot of years. It sounds a bit cheesy, but I’ve never wanted to be anything else. I count myself as being incredibly lucky, because I get excited about going to work every morning. I’m just coming into my thirty-fifth year working in addiction. With some of these patients, I know their families, they allow me to join in with their triumphs, commiserate with their sorrows, and it’s such a privilege.
During the outbreak, the nurses I manage were redeployed to the wards to do general nursing, and only myself and my deputy have stayed. We usually do lots of health promotion, but lots of our clients haven’t been allowed into the hospital, so we’ve only been dealing with people who are really sick.
Coronavirus has brought everyone together, people are going the extra mile, disputes are put aside. I’ve seen great acts of kindness, not only to patients, but also to each other. I’ve been really touched by this.
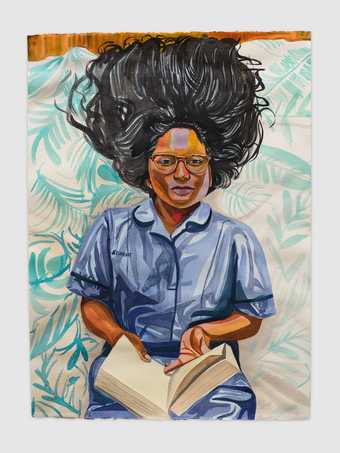
Team Time Storytelling, Alder Hey Children’s Hospital Emergency Department, Covid Pandemic 2020 Oil paint on canvas
Sitters left to right: Sarah, Jodie, Lalith, Jo, Claire, Kevin, Leah, Rose, Sue
Aliza Nisenbaum Team Time Storytelling, Steven Gerrard Garden, Alder Hey Children's Hospital Emergency Department, Covid Pandemic 2020 © Aliza Nisenbaum. Photography by Jeff McLane, courtesy the artist and Anton Kern Gallery, New York
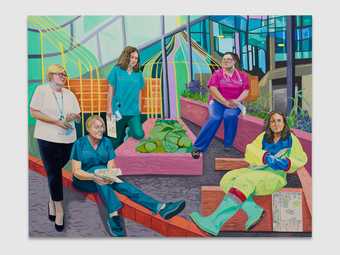
Sitters left to right: Amanda, Tracey, Charlotte, Leanne, Shirley
Team Time
These paintings portray a team from Alder Hey Children’s Hospital. Over these past months they have taken part in an initiative called Team Time, which focuses on staff wellbeing, using storytelling as a means of sharing emotional responses to situations at work. Reflecting the importance of play when working with children, each person was asked by Nisenbaum to make a drawing about their workplace experiences during the Covid-19 outbreak, and some of these are included within the paintings.
Sarah, Pathway Coordinator Team Leader
I’m a medical secretary, we’re called Pathway Coordinators at Alder Hey. We’re the first point of contact for most patients and we facilitate the pathway for patients’ treatment and care.
The build-up to Covid was hard. China and Italy were really suffering, but you’d think ‘it won’t get that bad here’, trying to stop yourself panicking. In work, we started getting constant emails about how we were preparing.
I was relieved when the schools closed. I really struggled sending my daughter in for the last couple of days, because I didn’t want to put her in danger. In mid-March, I started working from home, so I felt glad to be in a bubble with just myself and my family, and my stress calmed down. But you don’t want to speak to your family about Covid, because you want to shield them. Talking to colleagues helped, because it gave me a chance to speak to people who felt the same way.
Jodie, Senior Paediatric Nurse
I’m one of the senior nurses at the hospital in the emergency department, so I help to manage the staff who work alongside the doctors and the other nurses in the department.
Covid has made it tricky to communicate with people, because you have to wear face masks, and it’s really hard with children. They can’t see us smiling and that’s a massive part of communication. We haven’t been able to give hugs to people, if there’s a parent or family member that’s upset, we can’t offer them a hug, which is difficult.
Talking to other colleagues has been really nice, you talk about your experiences and realise that they feel the same, it makes you feel like you’re not alone. The team are all really lovely, it’s like a family.
Lalith, Consultant Physician
I am originally from Sri Lanka, but I was born and raised in Hong Kong and finished school in Beijing. What brought me to Merseyside was the Liverpool School of Tropical Medicine, where I did my master’s degree in global child health.
Something we’ve seen during the pandemic is that Covid-19 has not physically affected children as severely as adults, but lockdown and social distancing have nevertheless been detrimental to children’s physical and mental health. Closure of schools, restricted play and interaction with their peers, separation from extended family and socio-economic factors have impacted children and families on so many levels.
In the children's Emergency Department, we have seen an increase of accidents in the home, delayed presentations of new diagnoses of serious illnesses, as well as heart-wrenching cases of child abuse and mental health issues.
I was put in charge of staff wellbeing when lockdown was first announced in late March. I wanted to pilot Team Time as part of our wellbeing strategy and it has given us a chance to share stories that aren’t always heard, from our porters and secretaries, as well as the doctors and nurses. Our team is very important to me, so I wanted to promote principles of psychological first aid, and help my colleagues realise that they are not alone in how they feel.
Jo, Associate Director for Organisational Development and Consultant Psychologist
I’m a consultant clinical psychologist and my background is in child and adolescent mental health. I’ve been at Alder Hey for almost 15 years, and for the last 3 I’ve been working more in organisational psychology. This involves staff support and wellbeing, so anything to do with how it feels to work here. This has always been important, but during the Covid-19 pandemic it’s become even more prominent.
When I came into this role, the organisation had been going through a period of adversity. So I set up a staff advice and liaison service. This meant that staff members could talk to someone about their feelings and issues, either at work or at home. And we would either help directly or point people towards help. The need for this really accelerated once Covid hit. We have a drop-in facility in the hospital, so myself and my colleagues have been going in during the pandemic to continue running this.
Team Time sessions in the Emergency Department have been another key resource for staff wellbeing. This has provided a safe place for everyone in the department to be open with each other and has helped the team through some of their most challenging moments.
Claire, Healthcare Assistant
One of the good things during Covid is that we’ve got to spend lots of time with our children. We also got a new dog for our girls, and I don’t think that would have happened otherwise. But I have struggled with certain aspects and all the changes. We’re frontline workers, so we’ve worked all the way through. We also had to homeschool our children, and my eldest daughter lost her job. I’ve tried my best but I still felt that it wasn’t always good enough.
I work closely with the plastics team, dealing with facial injuries. That can be a very traumatic experience for the children. I’ve worked a lot with them, to help settle the children, and learning what the best outcome is for certain injuries. Our team has become one big family, and I think you really need to have each other’s backs.
Kevin, Hospital Porter
I’m a porter in Alder Hey children’s hospital, and my job is to transfer all the patients from department to department, ward to ward. Some of them are seriously injured, so we have to be very careful. We also move all the stock around the hospital. Sadly, children do die in A&E. This is especially hard for the young student nurses, they have never dealt with that, so I try to support them and tell them ‘don’t feel ashamed, let the tears flow, don’t bottle it up, when you go home, let it go’. When a child passes away, I go home and I raise a glass to them, that’s my way of coping.
As a porter, one of our jobs is to take patients to the mortuary. When Covid-19 really started we had twelve adults in our hospital, which is very rare, but one of our ICUs was used for adults only. I took one of them to the mortuary, and normally when a child passes away they are surrounded by their family, but in this case I was the only one accompanying them on their final journey which was very difficult.
Leah, Clinical Practice Educator
I have a dual nursing role at Alder Hey. Sometimes I’m out in A&E looking after the children directly, but I’m also the clinical educator for the department, meaning I’m responsible for staff training and professional development. We see so many varieties of illnesses and injuries in A&E that we joke that ‘accident and emergency’ should stand for ‘anything and everything’.
Covid has really changed things for us as a department. The number of patients dropped massively at the start of the outbreak. We were asking people to stay at home if they had Covid symptoms, but a lot of these symptoms are common childhood illnesses, so it’s been difficult finding the balance between who should stay at home and who needs to be seen by a clinician.
The pandemic has drastically changed how we work together, and the separation from family and friends has also been really difficult. We’ve felt isolated and separated from our normal lives, but thankfully we’ve had each other to keep ourselves going.
Rose, Health Play Specialist
I was in hospital a lot as a child, and when I was young, hospitals could be very unfriendly for children. After working in a few other jobs, I did my degree and decided I’d like to work in a hospital. I wanted a better time for the children. Every day in A&E I paint with them. I have some paintings that they’ve done for me, that’s when you know you’ve done something right, when a child gives you a picture.
I go to the operating theatre with the children and I also help keep them calm during invasive procedures like getting their blood taken. I have dreadful jokes that I tell. I’ll say things like ‘What does Father Christmas do to his elves when they’re naughty? He gives them the sack!’ They are bad, but they do the job for 8-year-olds!
We always put out toys in the waiting areas, but of course, we had to remove everything when Covid hit. We had to take away the games consoles, the toy boxes were emptied, no books or crayons, absolutely everything went. We also had to wear face masks, which stopped me blowing bubbles for the children. That’s a huge thing with the very young children, who can be frightened just of having their temperature taken.
I socialise a lot with friends, I have them over to stay at my little house. That’s something that’s changed a lot. I didn’t get my house until my late 50s, and it’s been really important to me, it’s got a nice little garden, friends come to stay. And all of a sudden, it became quite a sad little house, because nobody could come to stay.
Sue, Housekeeper
I’ve been working in Alder Hey for 19 years. I like the sound of the hustle and bustle, being on the go all the time.
At the start of lockdown, it was so quiet as people were scared to come into A&E. The days felt so long, which made the situation worse, you felt like you were waiting for something really bad to happen.
I look after all the stock, and it’s been a big responsibility looking after the PPE. It was daunting seeing colleagues getting dressed up in their PPE, it reminds you that their lives are at risk. So I’ve got to make sure that they’ve got the right equipment to stay safe.
By the time I got home from work, I was mentally drained and physically drained. I was waking up with anxiety, and my daughter was worried I was going to die, so that was upsetting. I’m not as anxious as I was, and I try to focus on the good things, but it’s in the back of your mind all the time. There was no way that I could work from home, I had to be on the forefront. But I am glad I’m part of it.
My brother has a serious illness affecting his immune system. I’ve been doing his shopping, putting it on his doorstep and talking to him from the gate. I like looking after people, it’s in my nature, it’s why I’m in the job.
Amanda, Head of Acute Care
I have been qualified for over 30 years and spent 27 of those within an acute paediatric setting. My current role is Head of Acute Care – essentially this is the lead nurse for the Emergency Department and assessment unit, general paediatric ward, diabetes team and the Acute Care Team. This means that I no longer work clinically, but I really enjoy people management in terms of support and staff development, particularly when you then watch those staff progress in their career or achieve their personal goals.
Covid has changed the way we all work. Every area has been affected by social distancing, PPE changes and requirements, or changing staffing levels. At the onset, getting the balance right was difficult as there were daily updates regarding process, training all the staff, and ensuring communications got to everyone. I felt like I was constantly at a planning event. I also couldn’t work as closely to support our staff, and at times that felt very isolating. I’m now on my own in my office, which can be great for getting work done, but it’s also lonely as most of my interaction with others is via the computer screen.
This has been a challenging time for the NHS, and something I’ve never really experienced in my career. I feel that the teams have really stepped up to the mark in dealing with everything expected of them, especially with all the constant changes.
Tracey, Paediatric Nurse Team Leader
I’ve worked as a nurse at Alder Hey for 20 years. I’m part of the infection control team and I got involved with Covid quite early, around January when it first started in China. My role was to train all the staff in the correct use of PPE. We’ve got around 60 of us in the nursing team, plus all the doctors, so it was quite a big task. I had to deliver something like 300 training sessions, which was quite daunting at first!
Back in summer last year I went to be trained at the infectious diseases unit at the adult hospital, and it was really helpful that I’d done that training before the Covid outbreak. I was the only one in my department who’d done this, so I felt it was my responsibility to get all my colleagues trained. I ended up making myself sick, as I’d worked so many hours and burned myself out. My colleagues were all very supportive, and if I had a problem, someone was always available for a chat.
Charlotte, Consultant Physician
I’m a consultant paediatrician and I’ve been working at Alder Hey for nearly 7 years. I work in the emergency department, so we see children with injuries or illness. With Covid, when it all started, we were worried that we were going to be overwhelmed with a huge number of patients, so we had to prepare for that. We sent out quite a lot of public health messages saying ‘if you don’t need to come to hospital, please stay at home’, which people did listen to. We initially went from a fairly normal, busy winter to sitting around with very few patients, which was really strange.
The biggest difficulty for us was the change in our policies and protocols, every day you would come in and something would have changed. It was quite emotionally exhausting trying to keep up with everything.
Another challenge is that we all wear the same blue scrubs, and we have to wear a mask all the time, so it can actually be really difficult to recognise people. It’s also been hard for the children. With the older ones, you can explain why you’re wearing a mask, but with some of the little ones, I’ve had a few who look absolutely terrified. You realise how much you usually use your facial expressions for communication.
Leanne, Advanced Paediatric Nurse
I originally qualified as a nurse in 2001 and went straight into the A&E department at Whiston Hospital. After doing my master’s degree, I moved to Alder Hey. I’ve been there for 3 years now.
My job is advanced paediatric nurse practitioner, so if you brought your child to A&E, you would either see a doctor or you’d see me. Parents are trusting you to look after their most precious thing, it’s such a big responsibility. You’re making massive decisions and ultimately parents are trusting that you’ve got the knowledge to make the clinical decisions. It’s a lovely job, it can be stressful at times, but it’s very rewarding.
At the beginning of the Covid outbreak, I was going into work and myself and my colleagues were terrified of bringing something home to our loved ones. But we’ve adapted well because in A&E, we’re trained in infection control and major incidents. My old boss once said to me ‘if you can work in A&E, you can work anywhere’. I think that’s right, you have to adapt very quickly and be able to think on your feet.
Shirley, Consultant Physician
I’m a Paediatric Emergency Medicine consultant, normally we would see a variety of patients, from minor illnesses or injuries, to very sick children with life threatening conditions. Covid-19 has changed my clinical role, physically, emotionally and mentally. Children and adults can carry the disease without showing any symptoms, and many of the symptoms are common things we see in children. So, I have to assume every patient might have it. Essentially, you think ‘this 5-year-old could make me seriously ill or even kill me’, something I’d never considered before.
School closure was the biggest challenge in my personal life. As a key worker, I was entitled to send my boys to school, but we opted to keep them at home. Home schooling was stressful, and I tried to be unphased when I saw other parents doing fun things with their children during lockdown. I also self-isolated at home for around a month and a half to avoid potentially infecting my family. This meant eating and sleeping in a different room and wearing a mask around the house. There were no hugs or cuddles with my boys. There is also the constant worry of not being able to visit my family in Malta, if they became unwell. Both of my siblings are in the medical profession, so like myself, they are at high risk of exposure.
Other works
Aliza Nisenbaum Susan, Aarti, Keerthana and Princess, Sunday in Brooklyn 2018 Oil on linen 145cm x 162.6cm Courtesy the artist and Anton Kern Gallery, New York/ © Aliza Nisenbaum
Susan, Aarti, Keerthana and Princess, Sunday in Brooklyn 2018
Nisenbaum first met Susan Shah in 2015 while undertaking a residency for Immigrant Women Leaders in New York. The two have kept in touch, and this painting is a result of their friendship. Susan is shown with her partner Aarti and their two daughters, a family with collective Indian and African American heritage who came together through immigration and adoption. Nisenbaum has said that they ‘are deeply committed to social justice and racial equity’ adding that ‘both women have devoted their careers to advancing education and human rights.’
Sitters from left to right: Susan Shah, Aarti Shah, Keerthana Shah, Princess Shah

Aliza Nisenbaum London Underground: Brixton Station and Victoria Line Staff 2018-19 Oil on polyester 190 x 361 cm Courtesy the artist and Art on the Underground, London; Mary Mary, Glasgow; Anton Kern Gallery, New York / © Aliza Nisebaum
London Underground: Brixton Staff and Victoria Line Staff 2019
Commissioned by Art on the Underground for Brixton station, Nisenbaum painted 15 people working for Transport for London in various roles on the Victoria Line. This included train drivers and operational staff, as well as people working in facilities and administration. She spent several hours getting to know each person as she painted them in her studio. Here, they are shown against a backdrop of iconic patterns from the London Underground, including the wall-tiles of Brixton station and the fabric design for the train seats on the Victoria Line.
Sitters from left to right: McKenzie Lawal, Cynthia Mason-Kalala, Jessica O’Gary, Patricia Osborne, Darrell McLeod, Ayesha Zafar Ahmad Kundi, Sylvia Enekeme, Adebukola Anifowose, Folasade Ogunro, Kay Ibrahim, Lydia Ward, James Daniel Betts, Anthony Joseph, Simon Austin, Robin Dixon

Aliza Nisenbaum Nimo, Sumiya, and Bisharo harvesting flowers and vegetables at Hope Community Garden 2017 Oil on linen
223.52 x 172.72 cm Courtesy the artist and Minneapolis Institute of Art, Minneapolis, Anton Kern Gallery, New York/ © Aliza Nisenbaum
Nimo, Sumiya, and Bisharo harvesting flowers and vegetables at Hope Community Garden 2017
In summer 2017, Nisenbaum undertook a 3-month residency at the Minneapolis Institute of Art. During this time, she worked closely with local community groups. Hope Community manages communal gardens and carries out food-related activities promoting health, culture, community and land stewardship. Nisenbaum painted three of the women who care for the gardens, these women represent two generations of Somali immigrants. Surrounded by symbols of sustenance and self-sufficiency, these women embody the bonds of care between family, friends, and community.
Sitters from left to right: Nimo Mohamed, Sumiya Olson, Bisharo Jama

Aliza Nisenbaum Morning Security Briefing at the Minneapolis Institute of Art, basement door open onto Guard Lounge Pet Wall 2017
Oil on linen 190cm x 240cm Courtesy the artist and Minneapolis Institute of Art, Minneapolis, Anton Kern Gallery, New York/ © Aliza Nisenbaum
Morning Security Briefing at the Minneapolis Institute of Art, basement door open onto the Guard Lounge Pet Wall 2017
The front of house team at MIA are the face of the museum, much like our own staff at Tate Liverpool. They play the vital role of facilitating the museum-going experience, as well as ensuring the safety of visitors and the artworks on display. During her residency at MIA, Nisenbaum befriended several of the museum guards. She learned about their hobbies, pets, and life stories during their time together in her studio.
Sitters from left to right: Jason Ressler, Desmond Griffin, Bruce Morrow, Katherine Lamb, Gina Carchedi, Jesse Nagamatsu

Aliza Nisenbaum Wise Elders Portraiture Class at Centro Tyrone Guzman with En Familia hay Fuerza, mural on the history of immigrant farm labor to the United States 2017 Oil on linen 190cm x 240cm Courtesy the artist and Minneapolis Institute of Art, Minneapolis, Anton Kern Gallery, New York/ © Aliza Nisenbaum
Wise Elders Portraiture Class at Centro Tyrone Guzman with En Familia hay Fuerza, mural on the history of immigrant farm labour to the United States 2017
During her time in Minneapolis, Nisenbaum taught a portrait drawing class as part of the Wise Elders programme at the Centro Tyrone Guzman. The programme supports the health and wellbeing of local Latino senior citizens. Here, the Wise Elders are shown with the drawings they made under Nisenbaum’s tutelage, while the mural in the background depicts the history of migrant labour in the Midwest US. The painting is a testament to them, their life experiences, and the collective wisdom they impart to their community.
Sitters from left to right: Melissa Benitez, Jesús Cazares, Sol, Juana Gonzales Moreno, Nicanor Torres Marcos, Minerva Cazares, Elena Valencia de los Santos, Roberto Arista